Referenties
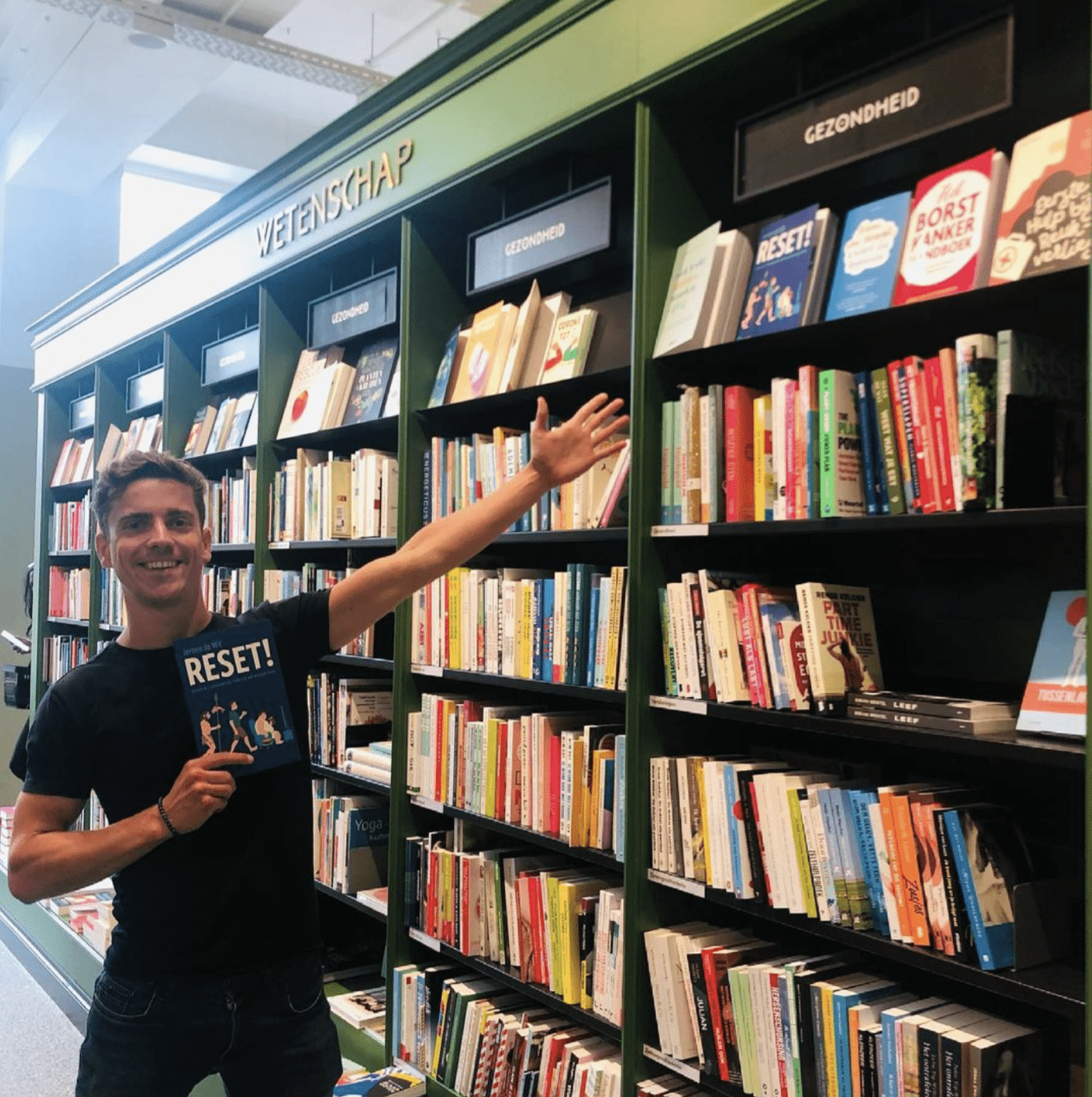
RESET! Ontdek de 5 elementen die leiden tot een energiek leven
351 referenties
- Ritchie, H. (2018, 14 februari). Causes of Death. Our World in Data. https://ourworldindata.org/causes-of-death
- Sioen, L. (2015, 25 april). ‘De planeet redt zichzelf wel. We moeten de mens redden’. De Standaard. https://www.standaard.be/cnt/dmf20150424_01647340
- Deze voetnoot bevat meerdere bronnen:
- Centraal Bureau voor de Statistiek. (2016, 25 januari). Meer dan 1 miljoen Nederlanders had depressie. https://www.cbs.nl/nl-nl/nieuws/2016/04/meer-dan-1-miljoen-nederlanders-had-depressie
- Overgewicht | Cijfers & Context | Huidige situatie | Volksgezondheidenzorg.info. (z.d.). Volksgezondheid & Zorg. Geraadpleegd op 12 juni 2020, van https://www.volksgezondheidenzorg.info/onderwerp/overgewicht/cijfers-context/huidige-situatie#!node-overgewicht-volwassenen
- info. (z.d.). Chronische aandoeningen en multimorbiditeit | Cijfers & Context | Huidige situatie | Volksgezondheidenzorg.info. Volksgezondheid & Zorg. Geraadpleegd op 12 juni 2020, van https://www.volksgezondheidenzorg.info/onderwerp/chronische-aandoeningen-en-multimorbiditeit/cijfers-context/huidige-situatie
- Centraal Bureau voor de Statistiek. (2020, 24 juni). StatLine – Gezonde levensverwachting vanaf 1981. https://opendata.cbs.nl/statline/#/CBS/nl/dataset/71950ned/table?ts=1614580556129
- (2019, 21 juni). Record: zorguitgaven Nederland naar 100 miljard euro. https://www.zorgwijzer.nl/zorgverzekering-2020/record-zorguitgaven-nederland-naar-100-miljard-euro
- Stanford Graduate School of Business. (2017, 13 november). Chamath Palihapitiya, Founder and CEO Social Capital, on Money as an Instrument of Change [Video]. https://www.youtube.com/watch?v=PMotykw0SIk
- MacKay, J. (2020, 20 februari). Screen time stats: How your phone impacts your workday – RescueTime. RescueTime Blog. https://blog.rescuetime.com/screen-time-stats-2018/
- Dunbar, R. I. M. (2009). The social brain hypothesis and its implications for social evolution. Annals of Human Biology, 36(5), 562–572. https://doi.org/10.1080/03014460902960289
- (2021, 28 januari). Number of global social network users 2017-2025. https://www.statista.com/statistics/278414/number-of-worldwide-social-network-users/
- Alhassan, A. A., Alqadhib, E. M., Taha, N. W., Alahmari, R. A., Salam, M., & Almutairi, A. F. (2018). The relationship between addiction to smartphone usage and depression among adults: a cross sectional study. BMC Psychiatry, 18(1), 1–2. https://doi.org/10.1186/s12888-018-1745-4
- (2019, 30 september). Which comes first: Smartphone dependency or depression?https://www.sciencedaily.com/releases/2019/09/190930161918.htm
- Lemola, S., Perkinson-Gloor, N., Brand, S., Dewald-Kaufmann, J. F., & Grob, A. (2014). Adolescents’ Electronic Media Use at Night, Sleep Disturbance, and Depressive Symptoms in the Smartphone Age. Journal of Youth and Adolescence, 44(2), 405–418. https://doi.org/10.1007/s10964-014-0176-x
- Violanti, J. M., & Marshall, J. R. (1996). Cellular phones and traffic accidents: An epidemiological approach. Accident Analysis & Prevention, 28(2), 265–270. https://doi.org/10.1016/0001-4575(95)00070-4
- Naumann, R. K., Ondracek, J. M., Reiter, S., Shein-Idelson, M., Tosches, M. A., Yamawaki, T. M., & Laurent, G. (2015). The reptilian brain. Current Biology, 25(8), R317–R321. https://doi.org/10.1016/j.cub.2015.02.049
- Ploog, D. W. (2003). The place of the Triune Brain in psychiatry. Physiology & Behavior, 79(3), 487–493. https://doi.org/10.1016/s0031-9384(03)00154-9
- Desbordes, G., Negi, L. T., Pace, T. W. W., Wallace, B. A., Raison, C. L., & Schwartz, E. L. (2012). Effects of mindful-attention and compassion meditation training on amygdala response to emotional stimuli in an ordinary, non-meditative state. Frontiers in Human Neuroscience, 6, 8–12. https://doi.org/10.3389/fnhum.2012.00292
- Lazar, S. W., Kerr, C. E., Wasserman, R. H., Gray, J. R., Greve, D. N., Treadway, M. T., McGarvey, M., Quinn, B. T., Dusek, J. A., Benson, H., Rauch, S. L., Moore, C. I., & Fischl, B. (2005). Meditation experience is associated with increased cortical thickness. NeuroReport, 16(17), 1893–1897. https://doi.org/10.1097/01.wnr.0000186598.66243.19
Resnick, B. (2016, 24 november). The myth of self-control. Vox. https://www.vox.com/science-and-health/2016/11/3/13486940/self-control-psychology-myth
- Eaton, S. B., Konner, M., & Shostak, M. (1988). Stone agers in the fast lane: Chronic degenerative diseases in evolutionary perspective. The American Journal of Medicine, 84(4), 739–749. https://doi.org/10.1016/0002-9343(88)90113-1
- Barker, G. (2009). The Agricultural Revolution in Prehistory: Why did Foragers become Farmers? (1ste editie, Vol. 1). Oxford, Engeland: Oxford University Press.
- Ashton, T. S. (1997). The Industrial Revolution 1760-1830 (2de editie, Vol. 2). Oxford, Verenigd Koninkrijk: Oxford University Press.
- Schoenherr, E. (2002, 14 februari). The Digital Revolution. Geraadpleegd op 15 juli 2020, van https://web.archive.org/web/20081007132355/http://history.sandiego.edu/gen/recording/digital.html
- Cohen, M. N., Armelagos, G. J., & Larsen, C. S. (2013). Paleopathology at the Origins of Agriculture (1ste editie, Vol. 1). Amsterdam, Nederland: Amsterdam University Press.
- Larsen, C. S. (2002). Skeletons in Our Closet: Revealing Our Past through Bioarchaeology (Revised editie, Vol. 1). Princeton, USA: Princeton University Press.
- Pinhasi, R., & Stock, J. T. (2010). Human Bioarchaeology of the Transition to Agriculture (1ste editie, Vol. 1). Hoboken, NJ, Verenigde Staten: Wiley.
- Cohen, M. N., & Crane-Kramer, G. M. M. (2012). Ancient Health: Skeletal Indicators of Agricultural and Economic Intensification (Bioarchaeological Interpretations of the Human Past: Local, Regional, and Global)(Reprint editie, Vol. 1). Florida, USA: University Press of Florida.
- Henneberg, M. (1988). Decrease of Human Skull Size in the Holocene. Human Biology, 60(3), 395–405. Geraadpleegd van https://www.jstor.org/stable/41464021
- Muskiet, F. (2008, 4 maart). nl – Onze voeding moet gebaseerd zijn op eetpatroon oermens. Geraadpleegd op 17 juli 2020, van https://www.plantaardigheden.nl/art_div/oermens.htm
- Angel, J. L. (1969). The bases of paleodemography. American Journal of Physical Anthropology, 30(3), 427–437. https://doi.org/10.1002/ajpa.1330300314
- Kaplan, H., Hill, K., Lancaster, J., & Hurtado, A. M. (2000). A theory of human life history evolution: Diet, intelligence, and longevity. Evolutionary Anthropology: Issues, News, and Reviews, 9(4), 156–185. https://doi.org/10.1002/1520-6505(2000)9:4
- Wenzel, G. W., Shephard, R. J., & Rode, A. (1997). The Health Consequences of “Modernization”: Evidence from Circumpolar Peoples. The Journal of the Royal Anthropological Institute, 3(1), 181. https://doi.org/10.2307/3034394
- Langbroek, M. (2004). `Out of Africa’: An investigation into the earliest occupation of the Old World (BAR International). In `Out of Africa’: An investigation into the earliest occupation of the Old World (BAR International) (1ste editie, Vol. 1, pp. 61–62). Londen, Engeland: British Archaeological Reports.
- Deze voetnoot bevat meerdere bronnen:
- Cowen, R. (2000). History of Life. In History of Life (2de editie, Vol. 1, pp. 363–364). Hoboken, NJ, Verenigde Staten: Wiley.
- Lewin, R. (2004). Human Evolution. In Human Evolution (1ste editie, Vol. 1, pp. 71–72). Hoboken, NJ, Verenigde Staten: Wiley.
- Aiello, L. C., & Wheeler, P. (1995). The Expensive-Tissue Hypothesis: The Brain and the Digestive System in Human and Primate Evolution. Current Anthropology, 36(2), 199–221. https://doi.org/10.1086/204350
- Milton, K. (2003). The Critical Role Played by Animal Source Foods in Human (Homo) Evolution. The Journal of Nutrition, 133(11), 3886S-3892S. https://doi.org/10.1093/jn/133.11.3886s
- Fonseca-Azevedo, K., & Herculano-Houzel, S. (2012). Metabolic constraint imposes tradeoff between body size and number of brain neurons in human evolution. Proceedings of the National Academy of Sciences, 109(45), 18571–18576. https://doi.org/10.1073/pnas.1206390109
- Crawford, M. A., Williams, G., Hassam, A. G., & Whitehouse, W. L. (1976). ESSENTIAL FATTY ACIDS AND FETAL BRAIN GROWTH. The Lancet, 307(7957), 452–453. https://doi.org/10.1016/s0140-6736(76)91476-8
- Burdge, G. C. (2006). Metabolism of α-linolenic acid in humans. Prostaglandins, Leukotrienes and Essential Fatty Acids, 75(3), 161–168. https://doi.org/10.1016/j.plefa.2006.05.013
- Cunnane, S. C., Ryan, M. A., Lin, Y. H., Lim, S.-Y., & Salem, N. (2006). Suckling Rats Actively Recycle Carbon from α-Linolenate into Newly Synthesized Lipids Even During Extreme Dietary Deficiency of n-3 Polyunsaturates. Pediatric Research, 59(1), 107–110. https://doi.org/10.1203/01.pdr.0000190569.07991.ed
- Mahaffey, K. R. (2004). Fish and shellfish as dietary sources of methylmercury and the ω-3 fatty acids, eicosahexaenoic acid and docosahexaenoic acid: risks and benefits. Environmental Research, 95(3), 414–428. https://doi.org/10.1016/j.envres.2004.02.006
- Stewart, K. M. (1994). Early hominid utilisation of fish resources and implications for seasonality and behaviour. Journal of Human Evolution, 27(1–3), 229–245. https://doi.org/10.1006/jhev.1994.1044
- Broadhurst, C. L., Cunnane, S. C., & Crawford, M. A. (1998). Rift Valley lake fish and shellfish provided brain-specific nutrition for early Homo. British Journal of Nutrition, 79(1), 3–21. https://doi.org/10.1079/bjn19980004
- Broadhurst, C. L., Wang, Y., Crawford, M. A., Cunnane, S. C., Parkington, J. E., & Schmidt, W. F. (2002). Brain-specific lipids from marine, lacustrine, or terrestrial food resources: potential impact on early African Homo sapiens. Comparative Biochemistry and Physiology Part B: Biochemistry and Molecular Biology, 131(4), 653–673. https://doi.org/10.1016/s1096-4959(02)00002-7
- Erlandson, J. M. (2010). Food for Thought: The Role of Coastlines and Aquatic Resources in Human Evolution. Human Brain Evolution, 125–136. https://doi.org/10.1002/9780470609880.ch7
- Kuipers, R. S., Joordens, J. C. A., & Muskiet, F. A. J. (2012). A multidisciplinary reconstruction of Palaeolithic nutrition that holds promise for the prevention and treatment of diseases of civilisation. Nutrition Research Reviews, 25(1), 96–129. https://doi.org/10.1017/s0954422412000017
- Braun, D. R., Harris, J. W. K., Levin, N. E., McCoy, J. T., Herries, A. I. R., Bamford, M. K., … Kibunjia, M. (2010). Early hominin diet included diverse terrestrial and aquatic animals 1.95 Ma in East Turkana, Kenya. Proceedings of the National Academy of Sciences, 107(22), 10002–10007. https://doi.org/10.1073/pnas.1002181107
- Brooks, A., Helgren, D., Cramer, J., Franklin, A., Hornyak, W., Keating, J., … et, A. L. (1995). Dating and context of three middle stone age sites with bone points in the Upper Semliki Valley, Zaire. Science, 268(5210), 548–553. https://doi.org/10.1126/science.7725099
- Wang, S., Lewis, C. M., Jakobsson, M., Ramachandran, S., Ray, N., Bedoya, G., … Ruiz-Linares, A. (2007). Genetic Variation and Population Structure in Native Americans. PLoS Genetics, 3(11), e185. https://doi.org/10.1371/journal.pgen.0030185
- Cunnane, S. C. (2005). Origins and evolution of the Western diet: implications of iodine and seafood intakes for the human brain. The American Journal of Clinical Nutrition, 82(2), 483. https://doi.org/10.1093/ajcn/82.2.483
- Service, R. F. (2017, 8 december). DNA could store all of the world’s data in one room. Geraadpleegd op 25 juli 2020, van https://www.sciencemag.org/news/2017/03/dna-could-store-all-worlds-data-one-room
- Clark, M. A., Choi, J. H., & Douglas, M. (2018). 16.3 Eukaryotic Epigenetic Gene Regulation. In Biology 2e (p. onbekend). Geraadpleegd van https://openstax.org/books/biology-2e/pages/16-3-eukaryotic-epigenetic-gene-regulation
- Deze voetnoot bevat meerdere bronnen:
- Klug, W. S., Cummings, M. R., Spencer, C. A., & Palladino, M. A. (2016). Essentials of Genetics, Global Edition. Londen, Engeland: Pearson Education Limited.
- Adams, J. U. (2008). Obesity, Epigenetics, and Gene Regulation. Geraadpleegd op 31 juli 2020, van https://www.nature.com/scitable/topicpage/obesity-epigenetics-and-gene-regulation-927/
- Strohman, R. C. (2003). Genetic Determinism as a Failing Paradigm in Biology and Medicine. Journal of Social Work Education, 39(2), 169–191. https://doi.org/10.1080/10437797.2003.10779130
- Hayashi, T., Urayama, O., Kawai, K., Hayashi, K., Iwanaga, S., Ohta, M., … Murakami, K. (2005). Laughter Regulates Gene Expression in Patients with Type 2 Diabetes. Psychotherapy and Psychosomatics, 75(1), 62–65. https://doi.org/10.1159/000089228
- Ornish, D., Magbanua, M. J. M., Weidner, G., Weinberg, V., Kemp, C., Green, C., … Carroll, P. R. (2008). Changes in prostate gene expression in men undergoing an intensive nutrition and lifestyle intervention. Proceedings of the National Academy of Sciences, 105(24), 8369–8374. https://doi.org/10.1073/pnas.0803080105
- Waterland, R. A., & Jirtle, R. L. (2003). Transposable Elements: Targets for Early Nutritional Effects on Epigenetic Gene Regulation. Molecular and Cellular Biology, 23(15), 5293–5300. https://doi.org/10.1128/mcb.23.15.5293-5300.2003
- Dolinoy, D. C., Huang, D., & Jirtle, R. L. (2007). Maternal nutrient supplementation counteracts bisphenol A-induced DNA hypomethylation in early development. Proceedings of the National Academy of Sciences, 104(32), 13056–13061. https://doi.org/10.1073/pnas.0703739104
- Weaver, I. C. G., Cervoni, N., Champagne, F. A., D’Alessio, A. C., Sharma, S., Seckl, J. R., … Meaney, M. J. (2004). Epigenetic programming by maternal behavior. Nature Neuroscience, 7(8), 847–854. https://doi.org/10.1038/nn1276
- Zhang, T. Y., Labonté, B., Wen, X. L., Turecki, G., & Meaney, M. J. (2012). Epigenetic Mechanisms for the Early Environmental Regulation of Hippocampal Glucocorticoid Receptor Gene Expression in Rodents and Humans. Neuropsychopharmacology, 38(1), 111–123. https://doi.org/10.1038/npp.2012.149
- University of Bristol. (2020, 27 oktober). Avon Longitudinal Study of Parents and Children | Avon Longitudinal Study of Parents and Children | University of Bristol. Geraadpleegd op 1 augustus 2020, van http://www.bristol.ac.uk/alspac/
- Oberlander, T. F., Weinberg, J., Papsdorf, M., Grunau, R., Misri, S., & Devlin, A. M. (2008). Prenatal exposure to maternal depression, neonatal methylation of human glucocorticoid receptor gene (NR3C1) and infant cortisol stress responses. Epigenetics, 3(2), 97–106. https://doi.org/10.4161/epi.3.2.6034
- Nerurkar, A., Bitton, A., Davis, R. B., Phillips, R. S., & Yeh, G. (2013). When Physicians Counsel About Stress: Results of a National Study. JAMA Internal Medicine, 173(1), 76. https://doi.org/10.1001/2013.jamainternmed.480
- Avey, H., Mathheny, K. B., Robbins, A., & Jackson, T. A. (2003). Health care providers’ training, perceptions, and practices regarding stress and health outcomes. JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION, 95(9), 833–845. https://pubmed.ncbi.nlm.nih.gov/14527051/
- Cummings, N. A., & Vandenbos, G. R. (1981). The twenty years Kaiser-Permanente experience with psychotherapy and medical utilization: implications for national health policy and national health insurance. Health Policy, 1(2), 159–175. https://pubmed.ncbi.nlm.nih.gov/10252343/
- Boron, W. B. F., & Boulapep, E. B. L. (2012). Concise Medical Physiology (1ste editie). Elsevier.
- Dhabhar, F. S. (2014). Effects of stress on immune function: the good, the bad, and the beautiful. Immunologic Research, 58(2–3), 193–210. https://doi.org/10.1007/s12026-014-8517-0
- LeBouef, T., Yaker, Z., & Whited, L. (2020, 1 juni). Physiology, Autonomic Nervous System. PubMed.https://www.ncbi.nlm.nih.gov/books/NBK538516/
- Bryan jr., R. M. (1990). Cerebral blood flow and energy metabolism during stress. American Journal of Physiology, 259–269. https://doi.org/10.1152/ajpheart.1990.259.2.H269
- Goosens, K. A. (2014). Opposing Effects of Chronic Stress on Amygdala and Hippocampus. Massachusetts Institute of Technology, onbekend. https://grantome.com/grant/NIH/R01-MH084966-01A1
- Lebedeva, A., Sundström, A., Lindgren, L., Stomby, A., Aarsland, D., Westman, E., Winblad, B., Olsson, T., & Nyberg, L. (2018). Longitudinal relationships among depressive symptoms, cortisol, and brain atrophy in the neocortex and the hippocampus. Acta Psychiatrica Scandinavica, 137(6), 491–502. https://doi.org/10.1111/acps.12860
- Vyas, A., Mitra, R., Shankaranarayana Rao, B. S., & Chattarji, S. (2002). Chronic Stress Induces Contrasting Patterns of Dendritic Remodeling in Hippocampal and Amygdaloid Neurons. The Journal of Neuroscience, 22(15), 6810–6818. https://doi.org/10.1523/jneurosci.22-15-06810.2002
- Sundermier, A. (2011, 15 maart). The particle physics of you. symmetry magazine. https://www.symmetrymagazine.org/article/the-particle-physics-of-you
- Porges, S. W. (2007). The polyvagal perspective. Biological Psychology, 74(2), 116–143. https://doi.org/10.1016/j.biopsycho.2006.06.009
- Porges, S. W. (2011). The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation (Norton Series on Interpersonal Neurobiology) (1ste editie). W. W. Norton & Company.
- Furness, J. B., & Poole, D. P. (2012). NONRUMINANT NUTRITION SYMPOSIUM: Involvement of gut neural and endocrine systems in pathological disorders of the digestive tract1,2. Journal of Animal Science, 90(4), 1203–1212. https://doi.org/10.2527/jas.2011-4825
- Gerritsen, R. J. S., & Band, G. P. H. (2018). Breath of Life: The Respiratory Vagal Stimulation Model of Contemplative Activity. Frontiers in Human Neuroscience, 12, evt. https://doi.org/10.3389/fnhum.2018.00397
Yackle, K., Schwarz, L. A., Kam, K., Sorokin, J. M., Huguenard, J. R., Feldman, J. L., Luo, L., & Krasnow, M. A. (2017). Breathing control center neurons that promote arousal in mice. Science, 355(6332), 1411–1415. https://doi.org/10.1126/science.aai7984
- (2017, 20 april). Nieuw rapport toont aan dat het tijd is voor verandering: gedragsverandering voor een duurzaam en gezond Europa | RIVM. https://www.rivm.nl/nieuws/nieuw-rapport-toont-aan-dat-tijd-is-voor-verandering-gedragsverandering-voor-duurzaam-en
- (1995). Dimensions of need: An atlas of food and agriculture. Food and Agriculture Organization of the United Nations.
- Masharani, U., Sherchan, P., Schloetter, M., Stratford, S., Xiao, A., Sebastian, A., Nolte Kennedy, M., & Frassetto, L. (2015). Metabolic and physiologic effects from consuming a hunter-gatherer (Paleolithic)-type diet in type 2 diabetes. European Journal of Clinical Nutrition, 69(8), 944–948. https://doi.org/10.1038/ejcn.2015.39
- Eaton, S. B., & Konner, M. (1985). Paleolithic Nutrition. New England Journal of Medicine, 312(5), 283–289. https://doi.org/10.1056/nejm198501313120505
- Cordain, L., Miller, J. B., Eaton, S. B., Mann, N., Holt, S. H. A., & Speth, J. D. (2000a). Plant-animal subsistence ratios and macronutrient energy estimations in worldwide hunter-gatherer diets. The American Journal of Clinical Nutrition, 71(3), 682–692. https://doi.org/10.1093/ajcn/71.3.682
- Kuipers, R. (2015). Het oerdieet (Vijfde druk). Bert Bakker.
- Cordain, L., Miller, J. B., Eaton, S. B., Mann, N., Holt, S. H. A., & Speth, J. D. (2000b). Plant-animal subsistence ratios and macronutrient energy estimations in worldwide hunter-gatherer diets. The American Journal of Clinical Nutrition, 71(3), 682–692. https://doi.org/10.1093/ajcn/71.3.682
- Kuipers, R. S., Luxwolda, M. F., Janneke Dijck-Brouwer, D. A., Eaton, S. B., Crawford, M. A., Cordain, L., & Muskiet, F. A. J. (2010). Estimated macronutrient and fatty acid intakes from an East African Paleolithic diet. British Journal of Nutrition, 104(11), 1666–1687. https://doi.org/10.1017/s0007114510002679
- Lee, R. B., & DeVore, I. (1968). Man the Hunter. Aldine.
- Cordain, L., Eaton, S. B., Sebastian, A., Mann, N., Lindeberg, S., Watkins, B. A., O’Keefe, J. H., & Brand-Miller, J. (2005). Origins and evolution of the Western diet: health implications for the 21st century. The American Journal of Clinical Nutrition, 81(2), 341–354. https://doi.org/10.1093/ajcn.81.2.341
- Rao, M., & Gershon, M. D. (2016). The bowel and beyond: the enteric nervous system in neurological disorders. Nature Reviews Gastroenterology & Hepatology, 13(9), 517–528. https://doi.org/10.1038/nrgastro.2016.107
- Mayer, E. A., Tillisch, K., & Gupta, A. (2015). Gut/brain axis and the microbiota. Journal of Clinical Investigation, 125(3), 926–938. https://doi.org/10.1172/jci76304
- Guinane, C. M., & Cotter, P. D. (2013). Role of the gut microbiota in health and chronic gastrointestinal disease: understanding a hidden metabolic organ. Therapeutic Advances in Gastroenterology, 6(4), 295–308. https://doi.org/10.1177/1756283×13482996
- Galland, L. (2014a). The Gut Microbiome and the Brain. Journal of Medicinal Food, 17(12), 1261–1272. https://doi.org/10.1089/jmf.2014.7000
- Het spijsverteringsstelsel bevat zo’n 39 triljoen bacteriën, vergeleken met 30 triljoen cellen in ons lichaam. (Sender, R., Fuchs, S., & Milo, R. (2016). Revised Estimates for the Number of Human and Bacteria Cells in the Body. PLOS Biology, 14(8), e1002533. https://doi.org/10.1371/journal.pbio.1002533)
- Evrensel, A., & Ceylan, M. E. (2016). Fecal Microbiota Transplantation and Its Usage in Neuropsychiatric Disorders. Clinical Psychopharmacology and Neuroscience, 14(3), 231–237. https://doi.org/10.9758/cpn.2016.14.3.231
- Rueda-Ruzafa, L., Cruz, F., Roman, P., & Cardona, D. (2019). Gut microbiota and neurological effects of glyphosate. NeuroToxicology, 75, 1–8. https://doi.org/10.1016/j.neuro.2019.08.006
- Xu, J., Huang, G., & Guo, T. (2016). Developmental Bisphenol A Exposure Modulates Immune-Related Diseases. Toxics, 4(4), 23. https://doi.org/10.3390/toxics4040023
- Chassaing, B., Van de Wiele, T., De Bodt, J., Marzorati, M., & Gewirtz, A. T. (2017). Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut, 66(8), 1414–1427. https://doi.org/10.1136/gutjnl-2016-313099
- Hruby, A., & Hu, F. B. (2014). The Epidemiology of Obesity: A Big Picture. PharmacoEconomics, 33(7), 673–689. https://doi.org/10.1007/s40273-014-0243-x
- Galland, L. (2014b). The Gut Microbiome and the Brain. Journal of Medicinal Food, 17(12), 1261–1272. https://doi.org/10.1089/jmf.2014.7000
- Van Ende, M., Wijnants, S., & Van Dijck, P. (2019). Sugar Sensing and Signaling in Candida albicans and Candida glabrata. Frontiers in Microbiology, 10, 99. https://doi.org/10.3389/fmicb.2019.00099
- Sandall, J., Tribe, R. M., Avery, L., Mola, G., Visser, G. H. A., Homer, C. S. E., Gibbons, D., Kelly, N. M., Kennedy, H. P., Kidanto, H., Taylor, P., & Temmerman, M. (2018). Short-term and long-term effects of caesarean section on the health of women and children. The Lancet, 392(10155), 1349–1357. https://doi.org/10.1016/s0140-6736(18)31930-5
- Westerfield, K. L., Koenig, K., & Oh, R. (2018). Breastfeeding: Common Questions and Answers. American Family Physician, 98(6), 368–373. https://www.aafp.org/afp/2018/0915/afp20180915p368.pdf
- Pannaraj, P. S., Li, F., Cerini, C., & et, A. L. (2017). Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatrics, 171(7), 647–654. https://doi.org/10.1001/jamapediatrics.2017.0378
- Singh, R. K., Chang, H.-W., Yan, D., Lee, K. M., Ucmak, D., Wong, K., Abrouk, M., Farahnik, B., Nakamura, M., Zhu, T. H., Bhutani, T., & Liao, W. (2017). Influence of diet on the gut microbiome and implications for human health. Journal of Translational Medicine, 15(1), 73. https://doi.org/10.1186/s12967-017-1175-y
- Leeming, E. R., Johnson, A. J., Spector, T. D., & Le Roy, C. I. (2019). Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients, 11(12), 2862. https://doi.org/10.3390/nu11122862
- Leff, J. W., & Fierer, N. (2013). Bacterial Communities Associated with the Surfaces of Fresh Fruits and Vegetables. PLoS ONE, 8(3), e59310. https://doi.org/10.1371/journal.pone.0059310
- Bell, V., Ferrão, J., Pimentel, L., Pintado, M., & Fernandes, T. (2018). One Health, Fermented Foods, and Gut Microbiota. Foods, 7(12), 195. https://doi.org/10.3390/foods7120195
- Karakan, T. (2020). Intermittent fasting and gut microbiota. The Turkish Journal of Gastroenterology, 30(12), 1008. https://doi.org/10.5152/tjg.2019.101219
- Craig, J. M., Logan, A. C., & Prescott, S. L. (2016). Natural environments, nature relatedness and the ecological theater: connecting satellites and sequencing to shinrin-yoku. Journal of Physiological Anthropology, 35(1), 1. https://doi.org/10.1186/s40101-016-0083-9
- Pennisi, E. (2020). Meet the ‘psychobiome’: the gut bacteria that may alter how you think, feel, and act. Science, 1. https://doi.org/10.1126/science.abc6637
- Eisenstein, M. (2020). The skin microbiome. Nature, 588(7838), S209. https://doi.org/10.1038/d41586-020-03523-7
- Rosenberg, E., & Zilber-Rosenberg, I. (2016). Do microbiotas warm their hosts? Gut Microbes, 7(4), 283–285. https://doi.org/10.1080/19490976.2016.1182294
- Tilg, H., Cani, P. D., & Mayer, E. A. (2016). Gut microbiome and liver diseases. Gut, 65(12), 2035–2044. https://doi.org/10.1136/gutjnl-2016-312729
- Belkaid, Y., & Hand, T. W. (2014). Role of the Microbiota in Immunity and Inflammation. Cell, 157(1), 121–141. https://doi.org/10.1016/j.cell.2014.03.011
- Tu, P., Chi, L., Bodnar, W., Zhang, Z., Gao, B., Bian, X., Stewart, J., Fry, R., & Lu, K. (2020). Gut Microbiome Toxicity: Connecting the Environment and Gut Microbiome-Associated Diseases. Toxics, 8(1), 19. https://doi.org/10.3390/toxics8010019
- Lee, C. J., Sears, C. L., & Maruthur, N. (2019a). Gut microbiome and its role in obesity and insulin resistance. Annals of the New York Academy of Sciences, 1461(1), 37–52. https://doi.org/10.1111/nyas.14107
- Ding, K., Hua, F., & Ding, W. (2020). Gut Microbiome and Osteoporosis. Aging and disease, 11(2), 438. https://doi.org/10.14336/ad.2019.0523
- Surin-Lord, S. (2020, 1 januari). The Microbiome’s Role In Common Hair Issues. HAPPI. https://www.happi.com/issues/2020-01-01/view_hairs-the-thing/the-microbiomes-role-in-common-hair-issues/
- Garnas, E. (2017, 30 mei). What Your Dreams Can Tell You About Your Microbiome. Darwinian Medicine. http://darwinian-medicine.com/what-your-dreams-can-tell-you-about-your-microbiome/
- Fetissov, S. O. (2016). Role of the gut microbiota in host appetite control: bacterial growth to animal feeding behaviour. Nature Reviews Endocrinology, 13(1), 11–25. https://doi.org/10.1038/nrendo.2016.150
- Pickard, J. M., Zeng, M. Y., Caruso, R., & Núñez, G. (2017). Gut microbiota: Role in pathogen colonization, immune responses, and inflammatory disease. Immunological Reviews, 279(1), 70–89. https://doi.org/10.1111/imr.12567
- Tang, W. H. W., Kitai, T., & Hazen, S. L. (2017). Gut Microbiota in Cardiovascular Health and Disease. Circulation Research, 120(7), 1183–1196. https://doi.org/10.1161/circresaha.117.309715
- Lee, C. J., Sears, C. L., & Maruthur, N. (2019b). Gut microbiome and its role in obesity and insulin resistance. Annals of the New York Academy of Sciences, 1461(1), 37–52. https://doi.org/10.1111/nyas.14107
- Shreiner, A. B., Kao, J. Y., & Young, V. B. (2015). The gut microbiome in health and in disease. Current Opinion in Gastroenterology, 31(1), 69–75. https://doi.org/10.1097/mog.0000000000000139
- Chakaroun, R. M., Massier, L., & Kovacs, P. (2020). Gut Microbiome, Intestinal Permeability, and Tissue Bacteria in Metabolic Disease: Perpetrators or Bystanders? Nutrients, 12(4), 1082. https://doi.org/10.3390/nu12041082
- Backhed, F., Ding, H., Wang, T., Hooper, L. V., Koh, G. Y., Nagy, A., Semenkovich, C. F., & Gordon, J. I. (2004). The gut microbiota as an environmental factor that regulates fat storage. Proceedings of the National Academy of Sciences, 101(44), 15718–15723. https://doi.org/10.1073/pnas.0407076101
- Silva, Y. P., Bernardi, A., & Frozza, R. L. (2020). The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Frontiers in Endocrinology, 11, 25. https://doi.org/10.3389/fendo.2020.00025
- Lustgarten, M. S. (2019). The Role of the Gut Microbiome on Skeletal Muscle Mass and Physical Function: 2019 Update. Frontiers in Physiology, 10, 1435. https://doi.org/10.3389/fphys.2019.01435
- Muskiet, F. A. J. (2011). De evolutionaire achtergrond, oorzaak en consequenties van chronische systemische lage graad ontsteking; betekenis voor de klinische chemie. Nederlands Tijdschrift Klinische Chemische Labgeneeskunde, 36(4), 199–214. https://www.nvkc.nl/sites/default/files/NTKC/Evolutionaireachtergrondchronischesystemischelagegraadontsteking_MuskietNTKC2011.pdf
- Nicholson, L. B. (2016). The immune system. Essays in Biochemistry, 60(3), 275–301. https://doi.org/10.1042/ebc20160017
- Bosma-den Boer, M. M., van Wetten, M.-L., & Pruimboom, L. (2012). Chronic inflammatory diseases are stimulated by current lifestyle: how diet, stress levels and medication prevent our body from recovering. Nutrition & Metabolism, 9(1), 32. https://doi.org/10.1186/1743-7075-9-32
- Fehm, H. L., Kern, W., & Peters, A. (2006). The selfish brain: competition for energy resources. Progress in Brain Research, 129–140. https://doi.org/10.1016/s0079-6123(06)53007-9
- Maffei, M., Halaas, J., Ravussin, E., Pratley, R. E., Lee, G. H., Zhang, Y., Fei, H., Kim, S., Lallone, R., Ranganathan, S., Kern, P. A., & Friedman, J. M. (1995b). Leptin levels in human and rodent: Measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nature Medicine, 1(11), 1155–1161. https://doi.org/10.1038/nm1195-1155
- Maffei, M., Halaas, J., Ravussin, E., Pratley, R. E., Lee, G. H., Zhang, Y., Fei, H., Kim, S., Lallone, R., Ranganathan, S., Kern, P. A., & Friedman, J. M. (1995a). Leptin levels in human and rodent: Measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nature Medicine, 1(11), 1155–1161. https://doi.org/10.1038/nm1195-1155
- Chan, J. L., Heist, K., DePaoli, A. M., Veldhuis, J. D., & Mantzoros, C. S. (2003). The role of falling leptin levels in the neuroendocrine and metabolic adaptation to short-term starvation in healthy men. Journal of Clinical Investigation, 111(9), 1409–1421. https://doi.org/10.1172/jci200317490
- Schwartz, M. W., Woods, S. C., Porte, D., Seeley, R. J., & Baskin, D. G. (2000). Central nervous system control of food intake. Nature, 404(6778), 661–671. https://doi.org/10.1038/35007534
- Friedman, J. M., & Halaas, J. L. (1998). Leptin and the regulation of body weight in mammals. Nature, 395(6704), 763–770. https://doi.org/10.1038/27376
- Dalamaga, M., Chou, S. H., Shields, K., Papageorgiou, P., Polyzos, S. A., & Mantzoros, C. S. (2013). Leptin at the Intersection of Neuroendocrinology and Metabolism: Current Evidence and Therapeutic Perspectives. Cell Metabolism, 18(1), 29–42. https://doi.org/10.1016/j.cmet.2013.05.010
- Allison, M. B., & Myers, M. G. (2014). 20 YEARS OF LEPTIN: Connecting leptin signaling to biological function. Journal of Endocrinology, 223(1), T25–T35. https://doi.org/10.1530/joe-14-0404
- Margetic, S., Gazzola, C., Pegg, G. G., & Hill, R. A. (2002). Leptin: a review of its peripheral actions and interactions. International Journal of Obesity, 26(11), 1407–1433. https://doi.org/10.1038/sj.ijo.0802142
- Wing, R., Sinha, M., Considine, R., Lang, W., & Caro, J. (1996). Relationship Between Weight Loss Maintenance and Changes in Serum Leptin Levels. Hormone and Metabolic Research, 28(12), 698–703. https://doi.org/10.1055/s-2007-979881
- Hinkle, W., Cordell, M., Leibel, R., Rosenbaum, M., & Hirsch, J. (2013). Effects of Reduced Weight Maintenance and Leptin Repletion on Functional Connectivity of the Hypothalamus in Obese Humans. PLoS ONE, 8(3), e59114. https://doi.org/10.1371/journal.pone.0059114
- Keim, N. L., Stern, J. S., & Havel, P. J. (1998). Relation between circulating leptin concentrations and appetite during a prolonged, moderate energy deficit in women. The American Journal of Clinical Nutrition, 68(4), 794–801. https://doi.org/10.1093/ajcn/68.4.794
- Ahima, R. S. (2008). Revisiting leptin’s role in obesity and weight loss. Journal of Clinical Investigation, 2380–2383. https://doi.org/10.1172/jci36284
- Spreadbury, I. (2012). Comparison with ancestral diets suggests dense acellular carbohydrates promote an inflammatory microbiota, and may be the primary dietary cause of leptin resistance and obesity. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, 175. https://doi.org/10.2147/dmso.s33473
- Pehrsson, P. R., Patterson, K. Y., Spungen, J. H., Wirtz, M. S., Andrews, K. W., Dwyer, J. T., & Swanson, C. A. (2016). Iodine in food- and dietary supplement–composition databases. The American Journal of Clinical Nutrition, 104(suppl_3), 868S-876S. https://doi.org/10.3945/ajcn.115.110064
- Broccoli bevat volgens het voedingscentrum (https://www.voedingscentrum.nl/nl/service/vraag-en-antwoord/gezonde-voeding-en-voedingsstoffen/hoeveel-calorieen-zitten-erin-/caloriechecker/brood-overige.aspx)1,6g vezels per 14kcal. Brood bevat volgens het voedingscentrum (https://www.voedingscentrum.nl/nl/service/vraag-en-antwoord/gezonde-voeding-en-voedingsstoffen/hoeveel-calorieen-zitten-erin-/caloriechecker/broccoli.aspx) 2,4g vezels per 139 kcal. Hierdoor bevat broccoli 1,6/14= 0,114g vezels per kcal en brood 2,4/139=0,017g vezels per kcal. 0,114/0,017=6,71 keer zoveel vezels in broccoli dan brood. Afgerond is dit 7.
- Logan, A. C. (2006). Dietary fiber, mood, and behavior. Nutrition, 22(2), 213–214. https://doi.org/10.1016/j.nut.2005.06.005
- Aune, D., Giovannucci, E., Boffetta, P., Fadnes, L. T., Keum, N. N., Norat, T., Greenwood, D. C., Riboli, E., Vatten, L. J., & Tonstad, S. (2017). Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—a systematic review and dose-response meta-analysis of prospective studies. International Journal of Epidemiology, 46(3), 1029–1056. https://doi.org/10.1093/ije/dyw319
- (z.d.-c). Welke noten zijn gezond om te eten? https://www.voedingscentrum.nl/nl/service/vraag-en-antwoord/gezonde-voeding-en-voedingsstoffen/welke-noten-zijn-goed-om-te-eten-.aspx
- Parnell, J., & A. Reimer, R. (2012). Prebiotic fiber modulation of the gut microbiota improves risk factors for obesity and the metabolic syndrome. Gut Microbes, 3(1), 29–34. https://doi.org/10.4161/gmic.19246
- SABATINO, A. D. I., MORERA, R., CICCOCIOPPO, R., CAZZOLA, P., GOTTI, S., TINOZZI, F. P., TINOZZI, S., & CORAZZA, G. R. (2005). Oral butyrate for mildly to moderately active Crohn’s disease. Alimentary Pharmacology and Therapeutics, 22(9), 789–794. https://doi.org/10.1111/j.1365-2036.2005.02639.x
- Dirt Poor: Have Fruits and Vegetables Become Less Nutritious? (2011, 27 april). Scientific American. https://www.scientificamerican.com/article/soil-depletion-and-nutrition-loss/
- Eng, M. (2018, 8 september). Most produce loses 30 percent of nutrients three days after harvest. chicagotribune.com. https://www.chicagotribune.com/dining/ct-xpm-2013-07-10-chi-most-produce-loses-30-percent-of-nutrients-three-days-after-harvest-20130710-story.html
- Lopresti, A. L. (2019). The Effects of Psychological and Environmental Stress on Micronutrient Concentrations in the Body: A Review of the Evidence. Advances in Nutrition, 103–112. https://doi.org/10.1093/advances/nmz082
- Coffey, D. S. (2001). Similarities of prostate and breast cancer: Evolution, diet, and estrogens. Urology, 57(4), 31–38. https://doi.org/10.1016/s0090-4295(00)00938-9
- Wassermann, B., Müller, H., & Berg, G. (2019). An Apple a Day: Which Bacteria Do We Eat With Organic and Conventional Apples? Frontiers in Microbiology, 10, 1629. https://doi.org/10.3389/fmicb.2019.01629
- Price-Pottenger Nutrition Foundation. (1988, 21 juni). MSG Dangers and Deceptions. Price-Pottenger. https://price-pottenger.org/journal_article/msg-dangers-and-deceptions/
- Heintze, E. (2019, 30 juni). MSG and its link to migraines. Starting Point Acupuncture & Wellness. https://startingpointacupuncture.com/msg-and-migraines/
- Polan, S. (2016, 5 september). Time for a Brake. Psychology Today. https://www.psychologytoday.com/us/articles/201609/time-brake
- Drago, S., El Asmar, R., Di Pierro, M., Grazia Clemente, M., Sapone, A. T. A., Thakar, M., Iacono, G., Carroccio, A., D’Agate, C., Not, T., Zampini, L., Catassi, C., & Fasano, A. (2006). Gliadin, zonulin and gut permeability: Effects on celiac and non-celiac intestinal mucosa and intestinal cell lines. Scandinavian Journal of Gastroenterology, 41(4), 408–419. https://doi.org/10.1080/00365520500235334
- Muskiet, F. A. J. (2011). De evolutionaire achtergrond, oorzaak en consequenties van chronische systemische lage graad ontsteking; betekenis voor de klinische chemie. Nederlands Tijdschrift Klinische Chemische Labgeneeskunde, 36(4), 199–214.
- Vojdani, A. (2015). agglutinins, and their roles in autoimmune reactivities. Alternative Therapy Health Med, 21(1), 46–51. https://pubmed.ncbi.nlm.nih.gov/25599185/
- Pruimboom, L., & de Punder, K. (2015a). The opioid effects of gluten exorphins: asymptomatic celiac disease. Journal of Health, Population and Nutrition, 33(1), 24. https://doi.org/10.1186/s41043-015-0032-y
- Cordain, L. (1999). Cereal Grains: Humanity’s Double-Edged Sword. Evolutionary Aspects of Nutrition and Health, 19–73. https://doi.org/10.1159/000059677
- Scant evidence of periodic starvation among hunter-gatherers. (1999). Diabetologia, 42(3), B383–B384. https://doi.org/10.1007/pl00002924
- Schlemmer, U., Frølich, W., Prieto, R. M., & Grases, F. (2009). Phytate in foods and significance for humans: Food sources, intake, processing, bioavailability, protective role and analysis. Molecular Nutrition & Food Research, 53(S2), S330–S375. https://doi.org/10.1002/mnfr.200900099
- Lopez, H. W., Krespine, V., Guy, C., Messager, A., Demigne, C., & Remesy, C. (2001). Prolonged Fermentation of Whole Wheat Sourdough Reduces Phytate Level and Increases Soluble Magnesium. Journal of Agricultural and Food Chemistry, 49(5), 2657–2662. https://doi.org/10.1021/jf001255z
- Jianqin, S., Leiming, X., Lu, X., Yelland, G. W., Ni, J., & Clarke, A. J. (2015). Effects of milk containing only A2 beta casein versus milk containing both A1 and A2 beta casein proteins on gastrointestinal physiology, symptoms of discomfort, and cognitive behavior of people with self-reported intolerance to traditional cows’ milk. Nutrition Journal, 15(1), 35. https://doi.org/10.1186/s12937-016-0147-z
- Farrell, H. M., Jimenez-Flores, R., Bleck, G. T., Brown, E. M., Butler, J. E., Creamer, L. K., Hicks, C. L., Hollar, C. M., Ng-Kwai-Hang, K. F., & Swaisgood, H. E. (2004). Nomenclature of the Proteins of Cows’ Milk—Sixth Revision. Journal of Dairy Science, 87(6), 1641–1674. https://doi.org/10.3168/jds.s0022-0302(04)73319-6
- Truswell, A. S. (2005). The A2 milk case: a critical review. European Journal of Clinical Nutrition, 59(5), 623–631. https://doi.org/10.1038/sj.ejcn.1602104
- Pruimboom, L., & de Punder, K. (2015b). The opioid effects of gluten exorphins: asymptomatic celiac disease. Journal of Health, Population and Nutrition, 33(1), 24. https://doi.org/10.1186/s41043-015-0032-y
- Bressan, P., & Kramer, P. (2016). Bread and Other Edible Agents of Mental Disease. Frontiers in Human Neuroscience, 10, 130. https://doi.org/10.3389/fnhum.2016.00130
- Dohan, F. C. (1988). Is schizophrenia rare if grain is rare? Bull., 14(4), 385–399. https://pubmed.ncbi.nlm.nih.gov/6609726/
- Wadley, G., & Martin, A. (1993). The origins of agriculture: A biological perspective and a new hypothesis. Journal of the Australasian College of Nutritional and Environmental Medicine, 6, 96–105. https://search.informit.org/doi/10.3316/INFORMIT.542636056785455
- Zaramela, L. S., Martino, C., Alisson-Silva, F., Rees, S. D., Diaz, S. L., Chuzel, L., Ganatra, M. B., Taron, C. H., Secrest, P., Zuñiga, C., Huang, J., Siegel, D., Chang, G., Varki, A., & Zengler, K. (2019). Gut bacteria responding to dietary change encode sialidases that exhibit preference for red meat-associated carbohydrates. Nature Microbiology, 4(12), 2082–2089. https://doi.org/10.1038/s41564-019-0564-9
- Kuipers, R. S., & Pruimboom, L. (2016). Short comment on “A review of potential metabolic etiologies of the observed association between red meat consumption and development of type 2 diabetes mellitus”, by Yoona Kim, Jennifer Keogh, Peter Clifton. Metabolism, 65(1), e3–e4. https://doi.org/10.1016/j.metabol.2015.09.006
- Hedlund, M., Padler-Karavani, V., Varki, N. M., & Varki, A. (2008). Evidence for a human-specific mechanism for diet and antibody-mediated inflammation in carcinoma progression. Proceedings of the National Academy of Sciences, 105(48), 18936–18941. https://doi.org/10.1073/pnas.0803943105
- Eleftheriou, P., Kynigopoulos, S., Giovou, A., Mazmanidi, A., Yovos, J., Skepastianos, P., Vagdatli, E., Petrou, C., Papara, D., & Efterpiou, M. (2014). Prevalence of Anti-Neu5Gc Antibodies in Patients with Hypothyroidism. BioMed Research International, 2014, 1–9. https://doi.org/10.1155/2014/963230
- ‘t Hart, B. A. (2015). Why does multiple sclerosis only affect human primates? Multiple Sclerosis Journal, 22(4), 559–563. https://doi.org/10.1177/1352458515591862
- Surette, M. E. (2008). The science behind dietary omega-3 fatty acids. Canadian Medical Association Journal, 178(2), 177–180. https://doi.org/10.1503/cmaj.071356
- (z.d.-b). Vis. Geraadpleegd op 29 juni 2020, van https://www.voedingscentrum.nl/encyclopedie/vis.aspx
- Hamilton, M. C., Hites, R. A., Schwager, S. J., Foran, J. A., Knuth, B. A., & Carpenter, D. O. (2005). Lipid Composition and Contaminants in Farmed and Wild Salmon. Environmental Science & Technology, 39(22), 8622–8629. https://doi.org/10.1021/es050898y
- Van Veen, P. A. F., & van der Sijs, N. (1997). Etymologisch woordenboek: de herkomst van onze woorden(2e druk). Van Dale Lexicografie.
- Halton, T. L., & Hu, F. B. (2004). The Effects of High Protein Diets on Thermogenesis, Satiety and Weight Loss: A Critical Review. Journal of the American College of Nutrition, 23(5), 373–385. https://doi.org/10.1080/07315724.2004.10719381
- Blom, W. A. M., Lluch, A., Stafleu, A., Vinoy, S., Holst, J. J., Schaafsma, G., & Hendriks, H. F. J. (2006). Effect of a high-protein breakfast on the postprandial ghrelin response. The American Journal of Clinical Nutrition, 83(2), 211–220. https://doi.org/10.1093/ajcn/83.2.211
- Mettler S., Mitchell N. & Tipton, K. (2010). Increased Protein Intake Reduces Lean Body Mass Loss during Weight Loss in Athletes. Medicine & Science in Sports & Exercise, 42(2), 326–337. https://doi.org/10.1249/mss.0b013e3181b2ef8e
- Bosse, J. D., & Dixon, B. M. (2012). Dietary protein to maximize resistance training: a review and examination of protein spread and change theories. Journal of the International Society of Sports Nutrition, 9(1), 42. https://doi.org/10.1186/1550-2783-9-42
- Russell, L. (2001). The importance of patients’ nutritional status in wound healing. British Journal of Nursing, 10(Sup1), S42–S49. https://doi.org/10.12968/bjon.2001.10.sup1.5336
- Kuipers, R. (2015). Het oerdieet (Vijfde druk). Bert Bakker.
- (z.d.-a). Eiwitten. Geraadpleegd op 29 juni 2020, van https://www.voedingscentrum.nl/encyclopedie/eiwitten.aspx#blok7
- Kabbouche, M. A., Powers, S. W., Vockell, A.-L. B., LeCates, S. L., Cfnp, & Hershey, A. D. (2003). Carnitine Palmityltransferase II (CPT2) Deficiency and Migraine Headache: Two Case Reports. Headache: The Journal of Head and Face Pain, 43(5), 490–495. https://doi.org/10.1046/j.1526-4610.2003.03095.x
- Marcovina, S. M., Sirtori, C., Peracino, A., Gheorghiade, M., Borum, P., Remuzzi, G., & Ardehali, H. (2013). Translating the basic knowledge of mitochondrial functions to metabolic therapy: role of L-carnitine. Translational Research, 161(2), 73–84. https://doi.org/10.1016/j.trsl.2012.10.006
- Mattson, M. P., Allison, D. B., Fontana, L., Harvie, M., Longo, V. D., Malaisse, W. J., Mosley, M., Notterpek, L., Ravussin, E., Scheer, F. A. J. L., Seyfried, T. N., Varady, K. A., & Panda, S. (2014). Meal frequency and timing in health and disease. Proceedings of the National Academy of Sciences, 111(47), 16647–16653. https://doi.org/10.1073/pnas.1413965111
- Barnosky, A. R., Hoddy, K. K., Unterman, T. G., & Varady, K. A. (2014). Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: a review of human findings. Translational Research, 164(4), 302–311. https://doi.org/10.1016/j.trsl.2014.05.013
- Longo, V. D., & Mattson, M. P. (2014). Fasting: Molecular Mechanisms and Clinical Applications. Cell Metabolism, 19(2), 181–192. https://doi.org/10.1016/j.cmet.2013.12.008
- Halberg, N., Henriksen, M., Söderhamn, N., Stallknecht, B., Ploug, T., Schjerling, P., & Dela, F. (2005). Effect of intermittent fasting and refeeding on insulin action in healthy men. Journal of Applied Physiology, 99(6), 2128–2136. https://doi.org/10.1152/japplphysiol.00683.2005
- Nair, K. S., Woolf, P. D., Welle, S. L., & Matthews, D. E. (1987). Leucine, glucose, and energy metabolism after 3 days of fasting in healthy human subjects. The American Journal of Clinical Nutrition, 46(4), 557–562. https://doi.org/10.1093/ajcn/46.4.557
- Zauner, C., Schneeweiss, B., Kranz, A., Madl, C., Ratheiser, K., Kramer, L., Roth, E., Schneider, B., & Lenz, K. (2000). Resting energy expenditure in short-term starvation is increased as a result of an increase in serum norepinephrine. The American Journal of Clinical Nutrition, 71(6), 1511–1515. https://doi.org/10.1093/ajcn/71.6.1511
Mansell, P. I., Fellows, I. W., & Macdonald, I. A. (1990). Enhanced thermogenic response to epinephrine after 48-h starvation in humans. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 258(1), R87–R93. https://doi.org/10.1152/ajpregu.1990.258.1.r87
- Orzeł-Gryglewska, J. (2010). Consequences of sleep deprivation. International Journal of Occupational Medicine and Environmental Health, 23(1), 95–114. https://doi.org/10.2478/v10001-010-0004-9
- Williamson, A. M. (2000). Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occupational and Environmental Medicine, 57(10), 649–655. https://doi.org/10.1136/oem.57.10.649
- Berkhout, K. (2018, 18 februari). Verslaafd aan een pilletje voor het slapen. NRC. https://www.nrc.nl/nieuws/2018/02/18/verslaafd-aan-een-pilletje-voor-het-slapen-a1592642
- Harmon, K., & Fu, Y. H. (2009, 13 augustus). Rare Genetic Mutation Lets Some People Function with Less Sleep. Scientific American. https://www.scientificamerican.com/article/genetic-mutation-sleep-less/
- Gallichio, L., & Kalesan, B. (2009). Sleep duration and mortality: a systematic review and meta-analysis. Journal of Sleep Research, 18(2), 148–158. https://doi.org/10.1111/j.1365-2869.2008.00732.x
- AlDabal, L. (2011a). Metabolic, Endocrine, and Immune Consequences of Sleep Deprivation. The Open Respiratory Medicine Journal, 5(1), 31–43. https://doi.org/10.2174/1874306401105010031
- Kloss, J. D., Perlis, M. L., Zamzow, J. A., Culnan, E. J., & Gracia, C. R. (2015). Sleep, sleep disturbance, and fertility in women. Sleep Medicine Reviews, 22, 78–87. https://doi.org/10.1016/j.smrv.2014.10.005
- Leproult, R. (2011). Effect of 1 Week of Sleep Restriction on Testosterone Levels in Young Healthy Men. JAMA, 305(21), 2173. https://doi.org/10.1001/jama.2011.710
- PhD, W. M. (2018). Why We Sleep: Unlocking the Power of Sleep and Dreams (Illustrated editie).
- Martin, B. J. (1981). Effect of sleep deprivation on tolerance of prolonged exercise. European Journal of Applied Physiology and Occupational Physiology, 47(4), 345–354. https://doi.org/10.1007/bf02332962
- Alhola, P., & Polo-Kantola, P. (2007). Sleep deprivation: Impact on cognitive performance. Neuropsychiatr Dis Treat., 3(5), 553–567. https://pubmed.ncbi.nlm.nih.gov/19300585/
- Bèchet, N. B., Shanbhag, N. C., & Lundgaard, I. (2020). Glymphatic function in the gyrencephalic brain. bioRxiv, nvt. https://doi.org/10.1101/2020.11.09.373894
- Iliff, J. J., Wang, M., Liao, Y., Plogg, B. A., Peng, W., Gundersen, G. A., Benveniste, H., Vates, G. E., Deane, R., Goldman, S. A., Nagelhus, E. A., & Nedergaard, M. (2012). A Paravascular Pathway Facilitates CSF Flow Through the Brain Parenchyma and the Clearance of Interstitial Solutes, Including Amyloid. Science Translational Medicine, 4(147), 147ra111. https://doi.org/10.1126/scitranslmed.3003748
- Goel, N., Rao, H., Durmer, J., & Dinges, D. (2009). Neurocognitive Consequences of Sleep Deprivation. Seminars in Neurology, 29(04), 320–339. https://doi.org/10.1055/s-0029-1237117
- Yoo, S.-S., Gujar, N., Hu, P., Jolesz, F. A., & Walker, M. P. (2007). The human emotional brain without sleep — a prefrontal amygdala disconnect. Current Biology, 17(20), R877–R878. https://doi.org/10.1016/j.cub.2007.08.007
- Gordon, A. M., & Chen, S. (2013). The Role of Sleep in Interpersonal Conflict. Social Psychological and Personality Science, 5(2), 168–175. https://doi.org/10.1177/1948550613488952
- Ezenwanne, E. (2011). Current concepts in the neurophysiologic basis of sleep; a review. Med Health Sci Res., 1(2), 173–179. https://pubmed.ncbi.nlm.nih.gov/23209972/
- Ridgeway, J., & French, C. (2012). Why did sleep evolve? Scientific American Mind, 23(6), 70. https://doi.org/10.1038/scientificamericanmind0113-70b
- Harbison, S. T. (2010). Evolution of Sleep: Phylogenetic and Functional Perspectives. Patrick McNamara, Robert A. Barton, and Charles L. Nunn, editors. Integrative and Comparative Biology, 50(4), 685–687. https://doi.org/10.1093/icb/icq053
- Jung, C. M., Melanson, E. L., Frydendall, E. J., Perreault, L., Eckel, R. H., & Wright, K. P. (2010). Energy expenditure during sleep, sleep deprivation and sleep following sleep deprivation in adult humans. The Journal of Physiology, 589(1), 235–244. https://doi.org/10.1113/jphysiol.2010.197517
- Marlowe, F. (2010). The Hadza (1ste editie). Amsterdam University Press.
- Susić, V. (2007). [Normal sleep]. Glas Srp Akad Nauka Med., 1–6. https://pubmed.ncbi.nlm.nih.gov/18069349/
- Maquet, P. A. A., Sterpenich, V., Albouy, G., Dang-Vu, T., Desseilles, M., Boly, M., Ruby, P., Laureys, S., & Peigneux, P. (2005). BRAIN IMAGING ON PASSING TO SLEEP. The Physiologic Nature of Sleep, 123–137. https://doi.org/10.1142/9781860947186_0006
- Parmeggiani, P. L., & Velluti, R. A. (2005). The Physiologic Nature of Sleep. In EEG, Polysomnography and other sleep recording systems (pp. 103–122). Amsterdam University Press.
- McCarley, R. W. (2007). Neurobiology of REM and NREM sleep. Sleep Medicine, 8(4), 302–330. https://doi.org/10.1016/j.sleep.2007.03.005
- Silber, M. H., Ancoli-Israel, S., Bonnet, M. H., Chokroverty, S., Grigg-Damberger, M. M., Hirshkowitz, M., Kapen, S., Keenan, S. A., Kryger, M. H., Penzel, T., Pressman, M. R., & Iber, C. (2007). The Visual Scoring of Sleep in Adults. Journal of Clinical Sleep Medicine, 03(02), 121–131. https://doi.org/10.5664/jcsm.26814
- Office of Communications and Public Liaison. (2017). Brain Basics: Understanding Sleep. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep
- Parmeggiani, P. L., & Velluti, R. A. (2005). The Physiologic Nature of Sleep. In EEG, Polysomnography and other sleep recording systems (pp. 103–122). Amsterdam University Press.
- Peever, J., & Fuller, P. M. (2016). Neuroscience: A Distributed Neural Network Controls REM Sleep. Current Biology, 26(1), R34–R35. https://doi.org/10.1016/j.cub.2015.11.011
- Walker, M. P., & van der Helm, E. (2009). Overnight therapy? The role of sleep in emotional brain processing. Psychological Bulletin, 135(5), 731–748. https://doi.org/10.1037/a0016570
- Garnas, E. (2017, 30 mei). What Your Dreams Can Tell You About Your Microbiome. Darwinian Medicine. http://darwinian-medicine.com/what-your-dreams-can-tell-you-about-your-microbiome/
- Greer, M. (2004). Strengthen your brain by resting it. American Psychological Association. https://www.apa.org/monitor/julaug04/strengthen
- Goode, E. (2001, 25 januari). Rats May Dream, It Seems, Of Their Days at the Mazes. The New York Times. https://www.nytimes.com/2001/01/25/us/rats-may-dream-it-seems-of-their-days-at-the-mazes.html
- Araujo, J. F., Patel, A. K., & Reddy, V. (2020, 29 april). Physiology, Sleep Stages. NCBI. https://www.ncbi.nlm.nih.gov/books/NBK526132/
- Milner, C. E., & Cote, K. A. (2009). Benefits of napping in healthy adults: Impact of nap length, time of day, age, and experience with napping. Journal of Sleep Research, 18(2), 272–281. https://doi.org/10.1111/j.1365-2869.2008.00718.x
- Mednick, S. C., Nakayama, K., Cantero, J. L., Atienza, M., Levin, A. A., Pathak, N., & Stickgold, R. (2002). The restorative effect of naps on perceptual deterioration. Nature Neuroscience, 5(7), 677–681. https://doi.org/10.1038/nn864
- Smolensky, M., & Lamberg, L. (2001). The Body Clock Guide to Better Health. Henry Holt and Company.
- Mohawk, J. A., Green, C. B., & Takahashi, J. S. (2012). Central and Peripheral Circadian Clocks in Mammals. Annual Review of Neuroscience, 35(1), 445–462. https://doi.org/10.1146/annurev-neuro-060909-153128
- Duffy, J. F., & Czeisler, C. A. (2009). Effect of Light on Human Circadian Physiology. Sleep Medicine Clinics, 4(2), 165–177. https://doi.org/10.1016/j.jsmc.2009.01.004
- Utiger, R. D. (1992). Melatonin — The Hormone of Darkness. New England Journal of Medicine, 327(19), 1377–1379. https://doi.org/10.1056/nejm199211053271909
- Falchi, F., Cinzano, P., Elvidge, C. D., Keith, D. M., & Haim, A. (2011). Limiting the impact of light pollution on human health, environment and stellar visibility. Journal of Environmental Management, 92(10), 2714–2722. https://doi.org/10.1016/j.jenvman.2011.06.029
- Love, T., Laier, C., Brand, M., Hatch, L., & Hajela, R. (2015). Neuroscience of Internet Pornography Addiction: A Review and Update. Behavioral Sciences, 5(3), 388–433. https://doi.org/10.3390/bs5030388
- Sofic, E., Rimpapa, Z., Kundurovic, Z., Sapcanin, A., Tahirovic, I., Rustembegovic, A., & Cao, G. (2005). Antioxidant capacity of the neurohormone melatonin. Journal of Neural Transmission, 112(3), 349–358. https://doi.org/10.1007/s00702-004-0270-4
- Zhang, D., Jones, R. R., James, P., Kitahara, C. M., & Xiao, Q. (2021). Associations between artificial light at night and risk for thyroid cancer: A large US cohort study. Cancer, nvt. https://doi.org/10.1002/cncr.33392
- Brain, M., Bryant, C. W., & Cunningham, M. (2020, 27 januari). How Caffeine Works. HowStuffWorks. https://science.howstuffworks.com/caffeine4.htm
- Okamoto-Mizuno, K., & Mizuno, K. (2012). Effects of thermal environment on sleep and circadian rhythm. Journal of Physiological Anthropology, 31(1), 14. https://doi.org/10.1186/1880-6805-31-14
- Obradovich, N., Migliorini, R., Mednick, S. C., & Fowler, J. H. (2017). Nighttime temperature and human sleep loss in a changing climate. Science Advances, 3(5), e1601555. https://doi.org/10.1126/sciadv.1601555
- Reilly, T. (1990). Human circadian rhythms and exercise. Critical Reviews in Biomedical Engineering, 18(3), 165–180. https://pubmed.ncbi.nlm.nih.gov/2286092/
- Youngstedt, S. D. (2005a). Effects of Exercise on Sleep. Clinics in Sports Medicine, 24(2), 355–365.https://doi.org/10.1016/j.csm.2004.12.003
- Takase, B., Akima, T., Uehata, A., Ohsuzu, F., & Kurita, A. (2004). Effect of chronic stress and sleep deprivation on both flow-mediated dilation in the brachial artery and the intracellular magnesium level in humans. Clinical Cardiology, 27(4), 223–227. https://doi.org/10.1002/clc.4960270411
- Abbasi, B., Kimiagar, M., Sadeghniiat, K., Shirazi, M., Hedeyati, M., & Rashidkhani, B. (2012). The effect of magnesium supplementation on primary insomnia in elderly: A double-blind placebo-controlled clinical trial. Journal of Research in Medical Sciences, 17(12), 1161–1169. https://pubmed.ncbi.nlm.nih.gov/23853635/
- (2019, 28 maart). How magnesium works – What magnesium does fundamentally. Magnesium.ca. http://www.magnesium.ca/how-magnesium-works/
- Jahangard, L., Sadeghi, A., Ahmadpanah, M., Holsboer-Trachsler, E., Sadeghi Bahmani, D., Haghighi, M., & Brand, S. (2018). Influence of adjuvant omega-3-polyunsaturated fatty acids on depression, sleep, and emotion regulation among outpatients with major depressive disorders – Results from a double-blind, randomized and placebo-controlled clinical trial. Journal of Psychiatric Research, 107, 48–56. https://doi.org/10.1016/j.jpsychires.2018.09.016
- Savage, K., Firth, J., Stough, C., & Sarris, J. (2017). GABA-modulating phytomedicines for anxiety: A systematic review of preclinical and clinical evidence. Phytotherapy Research, 32(1), 3–18. https://doi.org/10.1002/ptr.5940
- Youngstedt, S. D. (2005b). Effects of Exercise on Sleep. Clinics in Sports Medicine, 24(2), 355–365.https://doi.org/10.1016/j.csm.2004.12.003
Miller, D. J., Sargent, C., Roach, G. D., Scanlan, A. T., Vincent, G. E., & Lastella, M. (2019). Moderate-intensity exercise performed in the evening does not impair sleep in healthy males. European Journal of Sport Science, 20(1), 80–89. https://doi.org/10.1080/17461391.2019.1611934
- Marlowe, F. (2010). The Hadza (1ste editie). Amsterdam University Press.
- Nag, U. (2021, 23 februari). Usain Bolt record collection: the sprint king’s greatest hits. Olympic Channel. https://www.olympicchannel.com/en/stories/features/detail/usain-bolt-record-world-champion-athlete-fastest-man-olympics-sprinter-100m-200m/
- WHAT’S IT LIKE TO BE AN ANIMAL? (z.d.). Speed of Animals. http://www.speedofanimals.com/?u=m
- Schmidt-Nielsen, K. (1997). Temperature Regulation. In Animal Physiology: Adaptation and Environment (5de editie, p. 275). Cambridge University Press.
- Carrier, D. R., Kapoor, A. K., Kimura, T., Nickels, M. K., Scott, E. C., So, J. K., & Trinkaus, E. (1984). The Energetic Paradox of Human Running and Hominid Evolution [and Comments and Reply]. Current Anthropology, 25(4), 483–495. https://doi.org/10.1086/203165
- McCall, G. S. (2014). Before Modern Humans: New Perspectives on the African Stone Age (1ste editie).
- McDougall, C. (2011). Born to Run. Adfo Books.
- “Food For Thought” (PDF). The Life of Mammals.
- O’Keefe, J. H., Vogel, R., Lavie, C. J., & Cordain, L. (2010a). Organic Fitness: Physical Activity Consistent with our Hunter-Gatherer Heritage. The Physician and Sportsmedicine, 38(4), 11–18. https://doi.org/10.3810/psm.2010.12.1820
- Kuipers, R. (2015). Oergezond: word en blijf gezond met de oerleefstijl. Bert Bakker.
- O’Keefe, J. H., Vogel, R., Lavie, C. J., & Cordain, L. (2011). Exercise Like a Hunter-Gatherer: A Prescription for Organic Physical Fitness. Progress in Cardiovascular Diseases, 53(6), 471–479. https://doi.org/10.1016/j.pcad.2011.03.009
- Raichlen, D. A., Pontzer, H., Harris, J. A., Mabulla, A. Z. P., Marlowe, F. W., Josh Snodgrass, J., Eick, G., Colette Berbesque, J., Sancilio, A., & Wood, B. M. (2016). Physical activity patterns and biomarkers of cardiovascular disease risk in hunter-gatherers. American Journal of Human Biology, 29(2), e22919. https://doi.org/10.1002/ajhb.22919
- Nederlanders zitten veel, jongeren het meest. (2017, 11 juli). RIVM. https://www.rivm.nl/nieuws/nederlanders-zitten-veel-jongeren-meest
- Nomura, T., Yoshimoto, Y., Akezaki, Y., & Sato, A. (2008). Changing behavioral patterns to promote physical activity with motivational signs. Environmental Health and Preventive Medicine, 14(1), 20–25. https://doi.org/10.1007/s12199-008-0053-x
- Dell’Amore, C. (2021, 10 februari). Confirmed: Couch Potatoes Have Lower Sperm Counts. National Geographic. https://www.nationalgeographic.com/animals/article/130206-sperm-men-health-science-weird-sex
- Siddarth, P., Burggren, A. C., Eyre, H. A., Small, G. W., & Merrill, D. A. (2018). Sedentary behavior associated with reduced medial temporal lobe thickness in middle-aged and older adults. PLOS ONE, 13(4), e0195549. https://doi.org/10.1371/journal.pone.0195549
- Donnelly, L. (2019, 26 maart). Britain’s couch potato lifestyles could be causing 50,000 deaths a year. The Telegraph. https://www.telegraph.co.uk/news/2019/03/25/britains-couch-potato-lifestyles-could-causing-50000-deaths/
- Edwards, M. K., & Loprinzi, P. D. (2016). Sedentary behavior, physical activity and cardiorespiratory fitness on leukocyte telomere length. Health Promotion Perspectives, 7(1), 22–27. https://doi.org/10.15171/hpp.2017.05
- Bize, R., Johnson, J. A., & Plotnikoff, R. C. (2007). Physical activity level and health-related quality of life in the general adult population: A systematic review. Preventive Medicine, 45(6), 401–415. https://doi.org/10.1016/j.ypmed.2007.07.017
- Raichlen, D. A., Pontzer, H., Zderic, T. W., Harris, J. A., Mabulla, A. Z. P., Hamilton, M. T., & Wood, B. M. (2020). Sitting, squatting, and the evolutionary biology of human inactivity. Proceedings of the National Academy of Sciences, 117(13), 7115–7121. https://doi.org/10.1073/pnas.1911868117
- Davis, N. (2019, 14 januari). Moving every half hour could help limit effects of sedentary lifestyle, says study. the Guardian. https://www.theguardian.com/society/2017/sep/11/moving-every-half-hour-could-help-limit-effects-of-sedentary-lifestyle-says-study
- Hamblin, J. (2016, 17 augustus). Exercise Can’t Undo Sitting. The Atlantic. https://www.theatlantic.com/health/archive/2016/08/the-new-exercise-mantra/495908/
- S. Department of Health and Human Services. (2018). Physical Activity Guidelines for Americans (2de editie). https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf
- Wernbom, M., Augustsson, J., & Thome, R. (2007). The Influence of Frequency, Intensity, Volume and Mode of Strength Training on Whole Muscle Cross-Sectional Area in Humans. Sports Medicine, 37(3), 225–264. https://doi.org/10.2165/00007256-200737030-00004
- O’Keefe, J. H., Vogel, R., Lavie, C. J., & Cordain, L. (2010a). Organic Fitness: Physical Activity Consistent with our Hunter-Gatherer Heritage. The Physician and Sportsmedicine, 38(4), 11–18. https://doi.org/10.3810/psm.2010.12.1820
- Live and Let Die – the implications of cell death for health and illness. (2014). Karolinska Institutet. https://ki.se/en/research/live-and-let-die-the-implications-of-cell-death-for-health-and-illness
- Huang, S., & Czech, M. P. (2007). The GLUT4 Glucose Transporter. Cell Metabolism, 5(4), 237–252. https://doi.org/10.1016/j.cmet.2007.03.006
- Messina, G., Palmieri, F., & Monda, V. (2015). Exercise Causes Muscle GLUT4 Translocation in an Insulin-Independent Manner. Biology and Medicine, s3, 1–4. https://doi.org/10.4172/0974-8369.1000s3007
- Jensen, J., Rustad, P. I., Kolnes, A. J., & Lai, Y.-C. (2011). The Role of Skeletal Muscle Glycogen Breakdown for Regulation of Insulin Sensitivity by Exercise. Frontiers in Physiology, 2, 237–252. https://doi.org/10.3389/fphys.2011.00112
- Babyak, M., Blumenthal, J. A., Herman, S., Khatri, P., Doraiswamy, M., Moore, K., Edward Craighead, W., Baldewicz, T. T., & Ranga Krishnan, K. (2000). Exercise Treatment for Major Depression: Maintenance of Therapeutic Benefit at 10 Months. Psychosomatic Medicine, 62(5), 633–638. https://doi.org/10.1097/00006842-200009000-00006
- Josefsson, T., Lindwall, M., & Archer, T. (2013). Physical exercise intervention in depressive disorders: Meta-analysis and systematic review. Scandinavian Journal of Medicine & Science in Sports, 24(2), 259–272. https://doi.org/10.1111/sms.12050
- Scholz, J., Klein, M. C., Behrens, T. E. J., & Johansen-Berg, H. (2009). Training induces changes in white-matter architecture. Nature Neuroscience, 12(11), 1370–1371. https://doi.org/10.1038/nn.2412
- Pedersen, B. K., & Febbraio, M. A. (2008). Muscle as an Endocrine Organ: Focus on Muscle-Derived Interleukin-6. Physiological Reviews, 88(4), 1379–1406. https://doi.org/10.1152/physrev.90100.2007
- Hoon, M. W., Johnson, N. A., Chapman, P. G., & Burke, L. M. (2013a). The Effect of Nitrate Supplementation on Exercise Performance in Healthy Individuals: A Systematic Review and Meta-Analysis. International Journal of Sport Nutrition and Exercise Metabolism, 23(5), 522–532. https://doi.org/10.1123/ijsnem.23.5.522
- McMahon, N. F., Leveritt, M. D., & Pavey, T. G. (2016). The Effect of Dietary Nitrate Supplementation on Endurance Exercise Performance in Healthy Adults: A Systematic Review and Meta-Analysis. Sports Medicine, 47(4), 735–756. https://doi.org/10.1007/s40279-016-0617-7
- Hoon, M. W., Johnson, N. A., Chapman, P. G., & Burke, L. M. (2013a). The Effect of Nitrate Supplementation on Exercise Performance in Healthy Individuals: A Systematic Review and Meta-Analysis. International Journal of Sport Nutrition and Exercise Metabolism, 23(5), 522–532. https://doi.org/10.1123/ijsnem.23.5.522
- Grange, R. W., Isotani, E., Lau, K. S., Kamm, K. E., Huang, P. L., & Stul, J. T. (2015). Nitric oxide contributes to vascular smooth muscle relaxation in contracting fast-twitch muscles. JAMA Intern Med., 175(6), 970–977. https://doi.org/10.1152/physiolgenomics.2001.5.1.35
- Weitzberg, E., & Lundberg, J. O. N. (2002). Humming Greatly Increases Nasal Nitric Oxide. American Journal of Respiratory and Critical Care Medicine, 166(2), 144–145. https://doi.org/10.1164/rccm.200202-138bc
- Arem, H., Moore, S. C., Patel, A., Hartge, P., Berrington de Gonzalez, A., Visvanathan, K., Campbell, P. T., Freedman, M., Weiderpass, E., Adami, H. O., Linet, M. S., Lee, I.-M., & Matthews, C. E. (2015). Leisure Time Physical Activity and Mortality. JAMA Internal Medicine, 175(6), 959. https://doi.org/10.1001/jamainternmed.2015.0533
- Gebel, K., Ding, D., Chey, T., Stamatakis, E., Brown, W. J., & Bauman, A. E. (2015). Effect of Moderate to Vigorous Physical Activity on All-Cause Mortality in Middle-aged and Older Australians. JAMA intern Med., 175(6), 970–977. https://doi.org/10.1001/jamainternmed.2015.0541
- Mandolesi, L., Polverino, A., Montuori, S., Foti, F., Ferraioli, G., Sorrentino, P., & Sorrentino, G. (2018). Effects of Physical Exercise on Cognitive Functioning and Wellbeing: Biological and Psychological Benefits. Frontiers in Psychology, 9, 509. https://doi.org/10.3389/fpsyg.2018.00509
- Nieman, P. (2002). Psychosocial aspects of physical activity. Paediatrics and Child Health, 309–312. https://doi.org/10.1093/pch/7.5.309
Eime, R. M., Young, J. A., Harvey, J. T., Charity, M. J., & Payne, W. R. (2013). A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. International Journal of Behavioral Nutrition and Physical Activity, 10(1), 98. https://doi.org/10.1186/1479-5868-10-98
- Lacy, J. W., & Stark, C. (2013). The Neuroscience of Memory: Implications for the Courtroom. Nature reviews. Neuroscience, 14(9), 649–658. https://doi.org/10.1038/nrn3563
- Maria Millett, Michigan State University Extension. (2021, 25 januari). Challenge your negative thoughts. MSU Extension. https://www.canr.msu.edu/news/challenge_your_negative_thoughts
- Pert, C. B. (1999). Molecules Of Emotion: The Science Behind Mind-Body Medicine (1ste editie). Simon & Schuster.
- Etymology of “identity”. (2014, 13 februari). Textkit Greek and Latin Forums. https://www.textkit.com/greek-latin-forum/viewtopic.php?t=61102
- Postle, B. R. (2016). How Does the Brain Keep Information “in Mind”? Current Directions in Psychological Science, 25(3), 151–156. https://doi.org/10.1177/0963721416643063
- Cohen, C. C. H., Popovic, M. A., Klooster, J., Weil, M.-T., Möbius, W., Nave, K.-A., & Kole, M. H. P. (2020). Saltatory Conduction along Myelinated Axons Involves a Periaxonal Nanocircuit. Cell, 180(2), 311-322.e15. https://doi.org/10.1016/j.cell.2019.11.039
- Sharma, N., Classen, J., & Cohen, L. G. (2013). Neural plasticity and its contribution to functional recovery. Handb Clin Neurol, 110, 3–12. https://pubmed.ncbi.nlm.nih.gov/23312626/
- Kolb, B., Muhammad, A., & Gibb, R. (2011). Searching for factors underlying cerebral plasticity in the normal and injured brain. Journal of Communication Disorders, 44(5), 503–514. https://doi.org/10.1016/j.jcomdis.2011.04.007
- Berger, V. (2005). Understanding Frustration. Psychologist Anywhere Anytime. https://www.psychologistanywhereanytime.com/emotional_problems_psychologist/pyschologist_frustration.htm
- Nerurkar, A., Bitton, A., Davis, R. B., Phillips, R. S., & Yeh, G. (2013). When Physicians Counsel About Stress: Results of a National Study. JAMA Internal Medicine, 173(1), 76. https://doi.org/10.1001/2013.jamainternmed.480
- de Quervain, D. J.-F., Roozendaal, B., & McGaugh, J. L. (1998). Stress and glucocorticoids impair retrieval of long-term spatial memory. Nature, 394(6695), 787–790. https://doi.org/10.1038/29542
- Oei, N. Y. L., Elzinga, B. M., Wolf, O. T., de Ruiter, M. B., Damoiseaux, J. S., Kuijer, J. P. A., Veltman, D. J., Scheltens, P., & Rombouts, S. A. R. B. (2007). Glucocorticoids Decrease Hippocampal and Prefrontal Activation during Declarative Memory Retrieval in Young Men. Brain Imaging and Behavior, 1(1–2), 31–41. https://doi.org/10.1007/s11682-007-9003-2
- Kuhlmann, S. (2005). Impaired Memory Retrieval after Psychosocial Stress in Healthy Young Men. Journal of Neuroscience, 25(11), 2977–2982. https://doi.org/10.1523/jneurosci.5139-04.2005
- Morris, R. G. M., Garrud, P., Rawlins, J. N. P., & O’Keefe, J. (1982). Place navigation impaired in rats with hippocampal lesions. Nature, 297(5868), 681–683. https://doi.org/10.1038/297681a0
- Nasrallah, H. A. (2007). Remember the hippocampus!: You can protect the brain’s ‘regeneration center’. Current Psychiatry, 6(10), 17–18. https://www.mdedge.com/psychiatry/article/62883/remember-hippocampus-you-can-protect-brains-regeneration-center?sso=true
- Lipton, B. (2017). The jump from cell culture to consciousness. Integrative medicine, 16(6), 44–50. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6438088/
- Dijksterhuis, A., & Nordgren, L. F. (2006). A Theory of Unconscious Thought. Perspectives on Psychological Science, 1(2), 95–109. https://doi.org/10.1111/j.1745-6916.2006.00007.x
- Levy, B. R., Pilver, C., Chung, P. H., & Slade, M. D. (2014). Subliminal Strengthening. Psychological Science, 25(12), 2127–2135. https://doi.org/10.1177/0956797614551970
- Evans, J., & Budzynski, H. K. (2009). Introduction to Quantitative EEG and Neurofeedback (2de editie). Amsterdam University Press.
- Laibow R (2002) Personal Communication with BH Lipton. New Jersey, USA.
- Borjigin, J., Samantha Zhang, L., & Calinescu, A.-A. (2012). Circadian regulation of pineal gland rhythmicity. Molecular and Cellular Endocrinology, 349(1), 13–19. https://doi.org/10.1016/j.mce.2011.07.009
- Hamid, N. H. A., Sulaiman, N., Murat, Z. H., & Taib, M. N. (2015). Brainwaves stress pattern based on perceived stress scale test. 2015 IEEE 6th Control and System Graduate Research Colloquium (ICSGRC), 135–140. https://doi.org/10.1109/icsgrc.2015.7412480
- Korotkov, K. (2021). Where do we go? https://www.researchgate.net/publication/228784744_Where_Do_We_Go
- Hawkins, D. R. (2002). Power Vs.Force (Revised editie). Penguin Random House.
- SILVERTOOTH, E. W. (1986). Special relativity. Nature, 322(6080), 590. https://doi.org/10.1038/322590b0
- Michelson, A. A., & Morley, E. W. (1887). On the relative motion of the Earth and the luminiferous ether. American Journal of Science, s3-34(203), 333–345. https://doi.org/10.2475/ajs.s3-34.203.333
- Live and Let Die – the implications of cell death for health and illness. (2014). Karolinska Institutet. https://ki.se/en/research/live-and-let-die-the-implications-of-cell-death-for-health-and-illness
- How many chemical reactions occur in the human body per second? (2019). Brainly. https://brainly.in/question/9968664
- Li, C., Jiang, N., Wu, Y. K., Chang, W., Pu, Y. F., Zhang, S., & Duan, L. M. (2019). Quantum communication between multiplexed atomic quantum memories. Physical Review Letter, 124(4), 240504. https://doi.org/10.1103/PhysRevLett.124.240504
American Lung Association. (2017, 20 juli). How Your Lungs Get the Job Done. https://www.lung.org/blog/how-your-lungs-work
- Koenig, H. G. (2012). Religion, Spirituality, and Health: The Research and Clinical Implications. ISRN Psychiatry, 2012, 1–33. https://doi.org/10.5402/2012/278730
- Hilbert, M., & Lopez, P. (2011). The World’s Technological Capacity to Store, Communicate, and Compute Information. Science, 332(6025), 60–65. https://doi.org/10.1126/science.1200970
- Wells, D. (2017, 7 juli). Fun Facts About the Heart You Didn’t Know. Healthline. https://www.healthline.com/health/fun-facts-about-the-heart
- Witte, D. R., Grobbee, D. E., Bots, M. L., & Hoes, A. W. (2005). Excess cardiac mortality on Monday: the importance of gender, age and hospitalisation. European Journal of Epidemiology, 20(5), 395–399. https://doi.org/10.1007/s10654-004-6594-4
- Ohebsion, R. (z.d.). Native American Proverbs, Quotes, and Chants. Rodney Ohebsion. http://www.rodneyohebsion.com/native-american-proverbs-quotes.htm
- Ikeda, D. (2003). The Wisdom of the Lotus Sutra: A Discussion, Volume 6. World Tribune Press.
- Armour, J. A., & Ardell, J. L. (1994). Neurocardiology [E-book]. Institute of HeartMath. https://store.heartmath.org/e-Books/neurocardiology.html
- HeartMath Institute. (z.d.). Quick Coherence Technique for Adults. https://www.heartmath.org/resources/heartmath-tools/quick-coherence-technique-for-adults/
- Long, T. (2007, 12 maart). Patient Dies, but First Heart Transplant a Success. Wired. https://www.wired.com/2007/12/dayintech-1203/
- Sylvia, C., & Novak, W. (1998). A Change of Heart. Warner Books, New York.
- Pearsall, P. (1999). The Heart’s Code: Tapping the Wisdom and Power of Our Heart Energy (Reprint editie). Harmony.
- Gross, C. G. (1997). Leonardo da Vinci on the Brain and Eye. The Neuroscientist, 3(5), 347–355. https://doi.org/10.1177/107385849700300516
- McCraty, R., Atkinson, M., & Bradley, R. T. (2004). Electrophysiological Evidence of Intuition: Part 1. The Surprising Role of the Heart. The Journal of Alternative and Complementary Medicine, 10(1), 133–143. https://doi.org/10.1089/107555304322849057
- Boutin, C. (2006, 22 augustus). Snap judgments decide a face’s character, psychologist finds. Princeton University. https://www.princeton.edu/news/2006/08/22/snap-judgments-decide-faces-character-psychologist-finds?section=topstories
- McCraty, R. (2015). Science of the Heart – Exploring the Role of the Heart in Human Performance. Van Haren Publishing.
- Dispenza, J. (2019). Becoming Supernatural. Penguin Random House.
- The Math of HeartMath. (2014, 27 oktober). Heart Rate Variability. HeartMath Institute. https://www.heartmath.org/articles-of-the-heart/the-math-of-heartmath/heart-rate-variability/
- Alimujiang, A., Wiensch, A., Boss, J., Fleischer, N. L., Mondul, A. M., McLean, K., Mukherjee, B., & Pearce, C. L. (2019). Association Between Life Purpose and Mortality Among US Adults Older Than 50 Years. JAMA Network Open, 2(5), e194270. https://doi.org/10.1001/jamanetworkopen.2019.4270
- Einstein, Albert, brief aan Robert S. Marcus, politiek directeur van het World Jewish Congress, naar aanleiding van het overlijden van zijn zoon aan polio, 12 februari 1950.
- 1,01365=37,78
- Evans-Pritchard, B. (2013). Aiming To Reduce Cleaning Costs. Works That Work. https://worksthatwork.com/1/urinal-fly
- Richerson, P. J., & Boyd, O. P. R. (2006). Not by Genes Alone (New title editie). Amsterdam University Press.
- Morris, R. G. M. (2003). Long-term potentiation and memory. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences, 358(1432), 643–647. https://doi.org/10.1098/rstb.2002.1230

